While there are wounds that heal on their own without the need for dressing to help them heal, there are also those that require a dressing to allow them to heal properly and keep out elements that can cause the wound not to heal properly. The wound’s dressing allows the dead skin cells to collect in the dressing so that the wound can heal effectively.
Before the 1960s, clinicians have believed the perfect wound healing environment was dry and dressings simply plugged and concealed ulcers. However,it has confirmed by various studies in years that a moist wound environment where dressings have the opportunity to interact with the wound helped promote healing and reduced the risk of pain and infection while increasing outcomes.
The wet to dry dressing change is considered as an effective way to help wounds heal properly because the process allows a nurse to evaluate the wound for the signs and symptoms of various types of infections. It should be noted that it is the he patient’s doctor who will determine the schedule for the changing of wet to dry dressings.
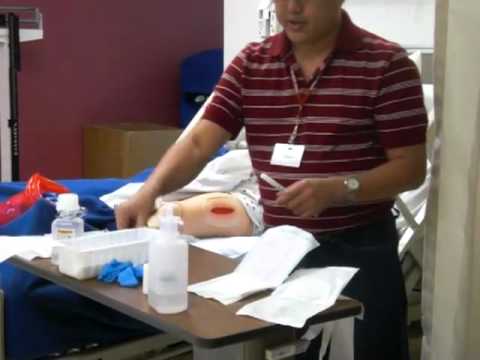
Dressing Changes: Sterile Technique
- Wash Hands
- Explain the procedure to the patient/caregiver
- Assemble the supplies at a convenient work area
- Assist the patient to a comfortable position to expose the wound. Place a plastic sheet under the patient to prevent soiling the linen. Drape the patient for privacy.
- Place a clean towel underneath the working area to minimize contamination.
- Open the sterile dressings, the irrigation and cleaning solution, and the instrument set to provide a sterile field.
- Wear a protective apron when caring for a patient with a draining wound. Don nonsterile gloves.
- Gently remove and discard the old tape and soiled dressing in a plastic trash bag. If the dressing sticks to the wound to the wound, moisten with sterile NSS and then remove.
- Remove and discard nonsterile gloves. Don sterile gloves.
- Cleanse and irrigate the wound as prescribed by the physician. Clean from the least contaminated area to the most contaminated area.
- Inspect the wound, and evaluate it for healing versus signs of infection.
- Apply a (moist) dressing,(gently feed moist gauze into the wound with cotton-tip applicators if packing is required)Place dry gauze over wet gauze. Then cover with a gauze dressing, ABD pad and secure it with hypoallergenic tape,Montgomery ties or a binder.
- Provide patient comfort measures.
- Clean and replace the equipment. Discard disposable items in a plastic trash bag.Close it securely, then put it in a second plastic bag, and close that bag securely. Put it in the trash.
- Wash your hands again when you are finished.
Tips on Changing a Wet to Dry Dressing
- Maintain a sterile setting by washing hands before and after dressing changes.
- Always check the patient’s charts to ensure the doctor ordered the dressing change. It is possible to cause additional medical issue by applying wet to dry dressing to certain wounds.
- Disposed of all old supplies and dressing in the appropriate areas to maintain a sterile environment.
- Use caution when removing old dressing because a new wound can delay the healing process of an existing wound.
- Any signs of infection, tissue loss, or excessive bleeding should be reported to the physician immediately.
Sources:
- https://www.scripps.org/articles/4275-wet-to-dry-dressing-changes
- https://www.registerednursern.com/wet-to-dry-dressing-how-to-change-a-wet-to-dry-dressing-clinical-nursing-skills/
- https://pennstatehershey.adam.com/content.aspx?productId=117&pid=60&gid=000315
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3601877/