Definition
- Removal of the entire contents of the eye within the scleral shell.
Discussion
- The sclera and muscles attached to the sclera remain intact to accommodate prosthesis.
- An indication for evisceration is a hopelessly traumatized eye in a young person with no history of previous eye disease.
- The cosmetic result is superior to the result of enucleation because the extrocular muscles remain attached to the scleral shell, resulting in a moveable implant very similar to that of natural eye movement.
Positioning
- Supine position, slightly elevated or flat.
- Arms are tucked and with soft restraints.
Drapes/ Packs
- Ophthalmic packs
- Special eye fenestrated sheet
- Basic pack
- Head or neck pack
Instrumentation
- Basic eye procedure tray
- Globe/ orbit prosthesis tray
- Curettes
Supplies/ Equipment
- Basin set
- Balanced saline solution
- Disposable cautery
- Ophthalmic sponges
- Suction tubing
- Antibiotic ophthalmic ointment
- Blade
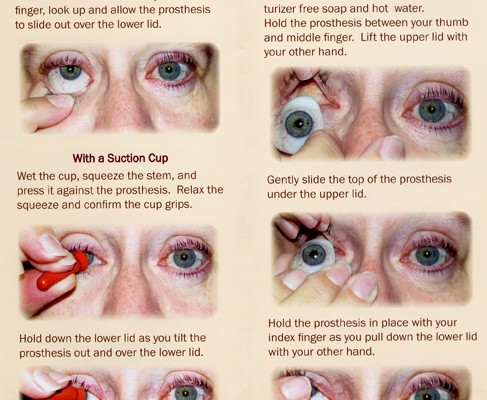
- Sphere prosthesis and conformer
Procedure
- A periotomy is made superiorly from the 3 o’ clock to the 9 o’clock position.
- An incision (same length) is made in the exposed sclera through to the uvea.
- The entire uvea is separated from the sclera by an evisceration spoon and is completely removed.
- The remaining uvea may be removed with a gauze sponge on a hemostat rotated within the scleral shell or with a special curetite.
- The wound is irrigated and hemostasis is achieved.
- The scleral edges are held open by tagged sutures while the implant is inserted with a sphere introducer.
- The posterior surface of the cornea is removed to reduce sensitivity, and the sclera is closed with interrupted sutures.
- The conjunctiva is approximated.
- A comformer is placed in the cul-de-sac.
- Antibiotic ointment is instilled and an eye pad and metal shield are applied.
Perioperative Nursing Consideration
- Have the prosthesis ready to implant.
- Follow hospital protocol regarding documentation of the prosthesis, and complete the enclosed manufacturer’s form.
- Strict aseptic technique during the entire procedure.
- Educate the patient about the changes and adjustment necessary after the procedure.








Gross
Where’s the gloves?
Is that a mummy?
No gloves!?
universal precaution.. remain sterile
Some psyche patients are doing it all by themselves
Be reasonable maybe the visual is done by the patient itself.
Gloves!!!!!
no sterile gloves?
Its not a moist eye socket that could get infected …the eye ball has been removed so basically the socket is only scar tissue.
Cool
Ugh,I hate anything with eyes!!! But with gloves anything is possible!!!
Lots of patients do it themselves. With no gloves. Obviously washing their hands prior to.
No sterile gloooves at all??
Do not assume that your patient has ever removed it themselves. My mom has had one for possibly close to 10 years, and it has only been removed once (as far as I can remember) outside of routine checkup/cleanings, and she didn’t remove it herself.
A major pet peeve of mine — a PERITOMY, not periotomy was made…
It is PERITOMY, not periotomy.