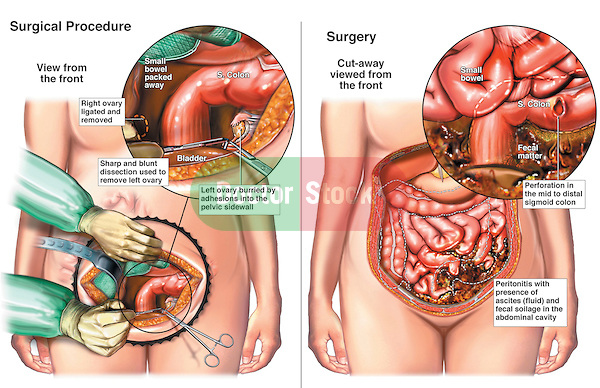
Bilateral Salpingo-oophorectomy with Perforation of the Colon. This medical illustration series shows an intra-operative view during a bilateral salpingo-oophorectomy surgery (removal of the ovaries). The second image reveals a post-operative bowel colon perforation and contamination of the abdomen by fecal contents.
- Monitor the patient’s blood pressure by arterial line if shock is present.
- Monitor consciousness
- Monitor central venous or pulmonary artery pressures and urine output frequently.
- Provide ongoing assessment of pain, GI function, and fluid and electrolyte balance.
- Assess nature of pain, location in the abdomen, and shifts of pain and location.
- Administer analgesic medication and position for comfort (eg, on side with knees flexed to decrease tension on abdominal organs).
- Record intake and output and CVP and/or pulmonary artery pressures.
- Administer and monitor IV fluids closely; nasogastric intubation may be necessary.
- Observe for decrease in temperature and pulse rate, softening of the abdomen, return of peristaltic sounds, and passage of flatus and bowel movements, which indicate peritonitis is subsiding.
- Increase food and oral fluids gradually, and decrease parenteral fluid intake when peritonitis subsides.
- Observe and record character of drainage from postoperative wound drains if inserted; take care to avoid dislodging drains.
- Postoperatively, prepare patient and family for discharge; teach care of incision and drains if still in place at discharge.
- Refer for home care if necessary.
Sources:
https://nurseslabs.com/peritonitis-nursing-management/
https://nanda-nursinginterventions.blogspot.com/2012/04/nursing-care-plan-for-peritonitis.html







