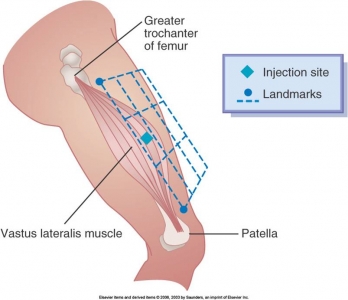
Vastus Lateralis Injection Site
Vastus Lateralis Injection Site
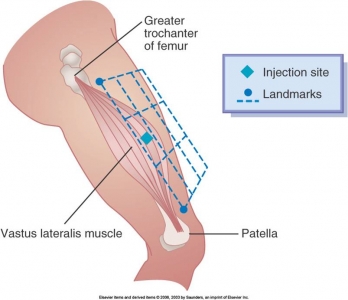
Vastus Lateralis Injection Site
[WATCH] Removing a NG (Nasogastric) Tube
Check physician’s order for removal of nasogastric tube.
Explain procedure to patient and assist to semi-Fowler’s position.
Gather equipment.
Perform hand hygiene. Don clean disposable gloves.
Place towel or disposable pad across patient’s chest. Give tissues to patient.
Discontinue suction and separate tube from suction. Unpin tube from patient’s gown and carefully remove adhesive tape from patient’s nose.
Attach syringe and flush with 10 mL normal saline solution or clean with 30 to 50 cc of air. (optional).
Instruct patient to take a deep breath and hold it.
Clamp tube with fingers by doubling tube on itself. Quickly and carefully remove tube while patient holds breath.
Place tube in disposable plastic bag. Remove gloves and place in bag.
Offer mouth care to patient and facial tissues to blow nose.
Measure nasogastric drainage. Remove all equipment and dispose according to agency policy. Perform hand hygiene.
Record removal of tube, patient’s response, and measure of drainage. Continue to monitor patient for 2 to 4 hours after tube removal for gastric distention, nausea, or vomiting.
Preparing Injections: Preparing Prefilled Medication Cartridge Syringes See also: How to Combine Two (2) Medications in One (1) Syringe

Withdrawing Venous Blood
PREPARING INJECTIONS 1. Check medication order. 2. Review pertinent information related to medication. 3. Assess client’s body build, muscle size, and weight. 4. Prepare medication:
[WATCH] How to do a Nasopharyngeal Suctioning
Determine need for suctioning. Administer pain medication before suctioning to postoperative patient.
Explain procedure to patient.
Assemble equipment.
Perform hand hygiene.
Adjust bed to comfortable working position. Lower side rail closet to you. Place patient in a semi-Fowler’s position if he or she is conscious. An unconscious patient should be placed in the lateral position facing you.
Place towel or waterproof pad across patient’s chest.
Turn suction to appropriate pressure.
https://nursingcrib.com/demo-checklist/suctioning-nasopharyngeal-and-oropharyngeal-areas/
Recent Comments