Assessment
- A thorough assessment of the skin is to be done annually on any individual with fair skin, frequent sun exposure, nevi, blemishes, freckles, skin discolorations, or those who have a history of malignant melanoma or other forms of skin cancer. Collaborate with other healthcare when examining the patient’s skin, ensure that all areas have been assessed.
- Interview patient or a family member regarding changes to the lesion or the appearance of a new pigmented lesion. An exam of the skin should include a numbering of moles, with documentation of their location, size, and appearance. Ask your patient whether moles or other lesions are painful or itch.
- Obtain a thorough history from your patient regarding the number of incidences of sunburn, the frequency of sun exposure, use of tanning beds, and a family history of melanoma.
Nursing Care
If surgical removal was performed:
- Inspect the incision for signs of infection or bleeding and monitor the amount, odor, and consistency of drainage on the wound dressing.
- Antibiotic therapy is often prescribed to prevent post-op infection.
For graft
- Assess the donor site for bleeding and infection.
- Carefully clean the skin with antimicrobial soap and water using sterile gauze.
- Be sure not to get the skin graft or donor site wet.
- Protect the skin graft and donor site from overexposure to light sources, including the sun, to prevent burning or blistering.
- Don’t forget to manage the patient’s pain due to wide and deep excision of the melanoma.
For radiation therapy
- Assess the skin over the treatment area for redness, irritation, or signs of infection.
- Avoid using creams or lotions and protect the skin from light sources.
- Conserve your patient’s energy as much as possible because radiation therapy tends to cause fatigue.
- Don’t forget to assess your patient for signs and symptoms of infection secondary to immunotherapy or chemotherapy.
- Trend the WBC count and differential for any indications of infection.
- Be sure to provide emotional support for your patient.
- Encourage your patient to become involved in support groups or counseling.
Patient Teaching about early detection
- Teach your patient that regular skin self-exam and assessments by the healthcare provider are especially important for people who have a higher than normal risk for malignant melanoma.
- Teach your patient to assess the skin thoroughly, especially if there’s a family history of malignant melanoma.
- Advise the patient that the best time to perform a skin self-exam is after a shower or bath. The skin should be checked in a well-lit room using a full-length mirror and handheld mirror while being completely naked.
- Tell your patient to check all areas of the skin, including but not limited to the back, face, scalp, between the buttocks, under the breasts, the soles of the feet, and the genital area.
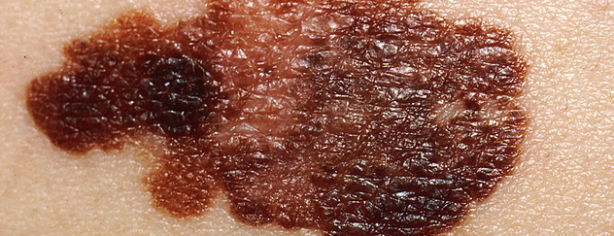
- Explain to your patient that he’s looking for a new mole; a mole that looks abnormal; a change in the size, shape, color, or texture of a mole or birthmark; or a sore that doesn’t heal.
- Don’t forget to teach your patient’s spouse or partner about melanoma and other forms of skin cancer.
- Changes in the skin are sometimes initially identified by a patient’s spouse during intimacy or daily activities.
- Changes in the skin must be promptly reported to the healthcare provider.
- Teach your patient about the ABCDEs of melanoma lesions, stress the importance of minimizing exposure to the sun, and encourage your patient and family members to learn more about melanoma.
Source:
https://www.nursingcenter.com/journalarticle?Article_ID=1100773